Read the Latest Sleep News and find your Adelaide sleep specialist here!
Here you’ll find the latest sleep news about Sleep Disorders, and innovations in Sleep medicine
Our blog and news feed is ever increasing, and now covers :
Obstructive Sleep Apnoea (OSA) and it’s effects on your body
OSA contributes to Hypertension / high blood pressure
Sleep Apnea and Glaucoma, erectile dysfunction, memory loss, strokes / CVAs
OSA and cardiovascular disease (including Atrial Fibrillation, AF)
Sleepwalking, sleeptalking and REM Behavior Disorder (RBD)
Sleep Apnea can worsen your diabetes
Untreated Sleep Apnoea is costing you financially
Fixing sleep in Teenagers and Adolescents
RLS and Gambling, Impulsive Behaviours
Memory loss and poor concentration
CPAP prevents Atrial Fibrillation recurrence in those with OSA
Blue light and body clocks
Worldwide recall of ASV machines
OSA and depression
Congenital Long QT Syndrome
45% of those with heart disease have OSA
Cancer incidence and OSA
CPAP and lowering car accident risk
REM-OSA and Hypertension
. . . AND MORE!
There is a whole world of other sleep disorders, including Narcolepsy, Idiopathic Hypersomnia, Restless Legs Syndrome (RLS), Delayed Sleep Phase and Free Running Rhythm, other Circadian Rhythm Disturbances, Insomnia, and so much more.
You’ll also be able to read about the treatments available – from machines such as Continuous Positive Airways Pressure (CPAP) and Bilevel PAP (BiPAP), to medications such as Modafinil, Armodafinil, Dexamphetamine, Sodium Oxybate (Xyrem), Pramipexole (Sifrol) and so much more.
Our Sleep doctors are experts in all of these conditions, and all of these treatments. We also see Teenagers and Adolescents, not just Adults. We hope you’ll find our blog useful.
The treatment of Narcolepsy including Sodium Oxybate (Xyrem) and Modafinil
Narcolepsy is one of the most complex of non-respiratory Sleep Disorders, consisting of a tetrad of Excessive Daytime Sleepiness,
The Diagnosis of Narcolepsy and the MSLT
Narcolepsy is one of the most interesting of Sleep Disorders in the International Classification of Sleep Disorders (ICSD-3). It is
The History of Narcolepsy – Excessive sleepiness in evolution
Central Disorders of Hypersomnolence encompass conditions including Narcolepsy and Idiopathic Hypersomnia - at here at the best Adelaide Sleep
2017 Nobel prize winners : the first to be awarded in the field of Sleep Medicine!
Congratulations to the 2017 Nobel Prize Winners in Physiology or Medicine : Jeffrey C. Hall, Michael Rosbash and Michael
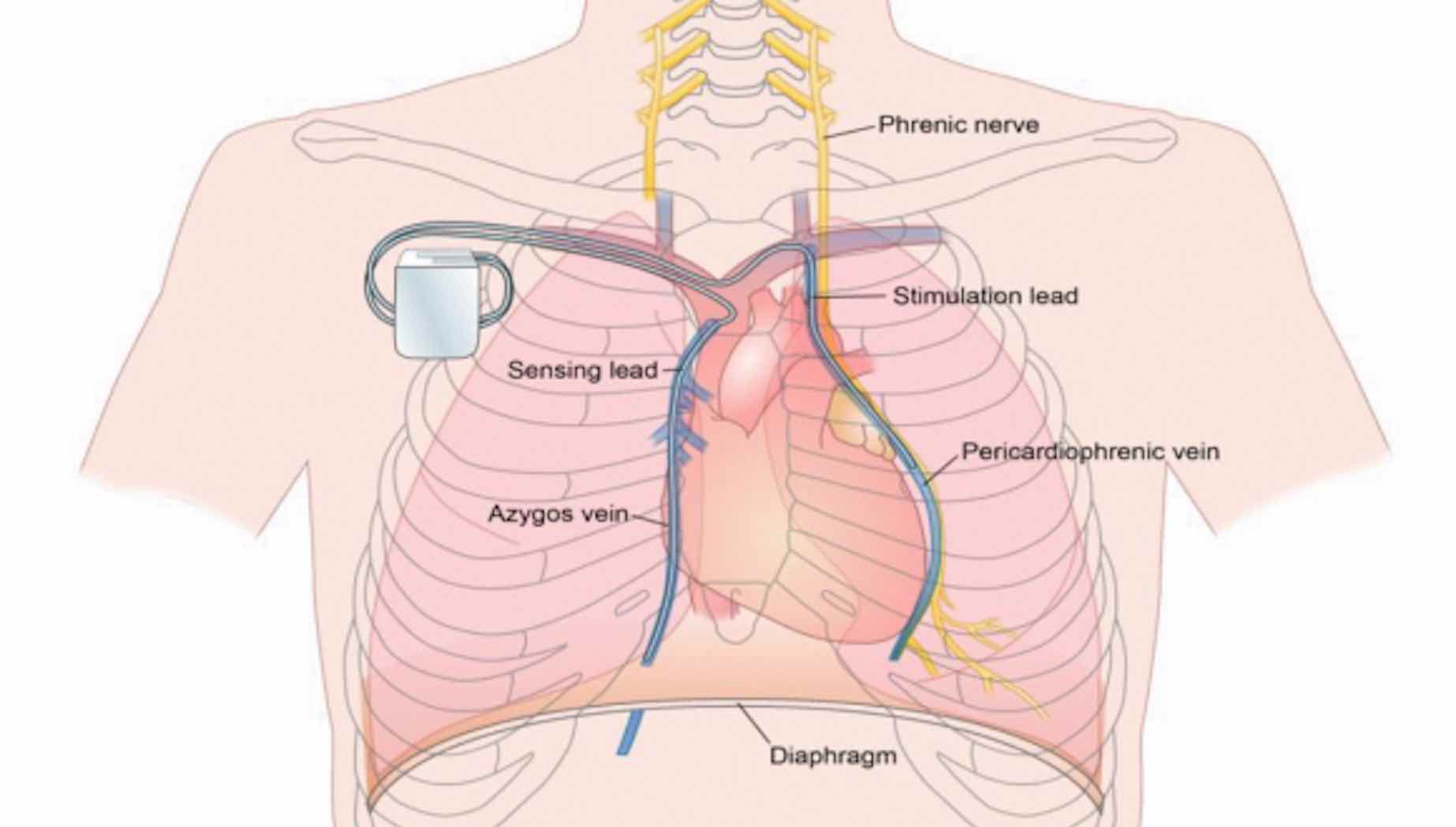
Diaphragm pacing for Central Sleep Apnoea
Treatments for Central Sleep Apnoea (CSA) are limited - that's why we're excited about the potential for new treatments
Showcasing the Burnside Sleep Centre
Your sleep study produces over 1,000 pages of data - and that's why we prefer a local Adelaide centre
Does REM-dependent OSA matter? In Blood pressure, it does!
Whilst we know that Severe OSA is associated with cardiovascular risk, a significant ‘grey area’ exists. This grey area
Rapid access to a sleep study
We’re delighted to announce that our Adelaide Sleep clinic and sleep study services have been extended! We now
CPAP for OSA can lower the risk of Car Accidents
There is a wealth of data that acknowledges poor sleep (namely poor sleep due to Obstructive Sleep Apnoea (OSA))
Cancer and OSA – an unlikely link?
Does having Severe OSA increase your risk of Cancer? Looking back on the years of Obstructive Sleep Apnoea (OSA)
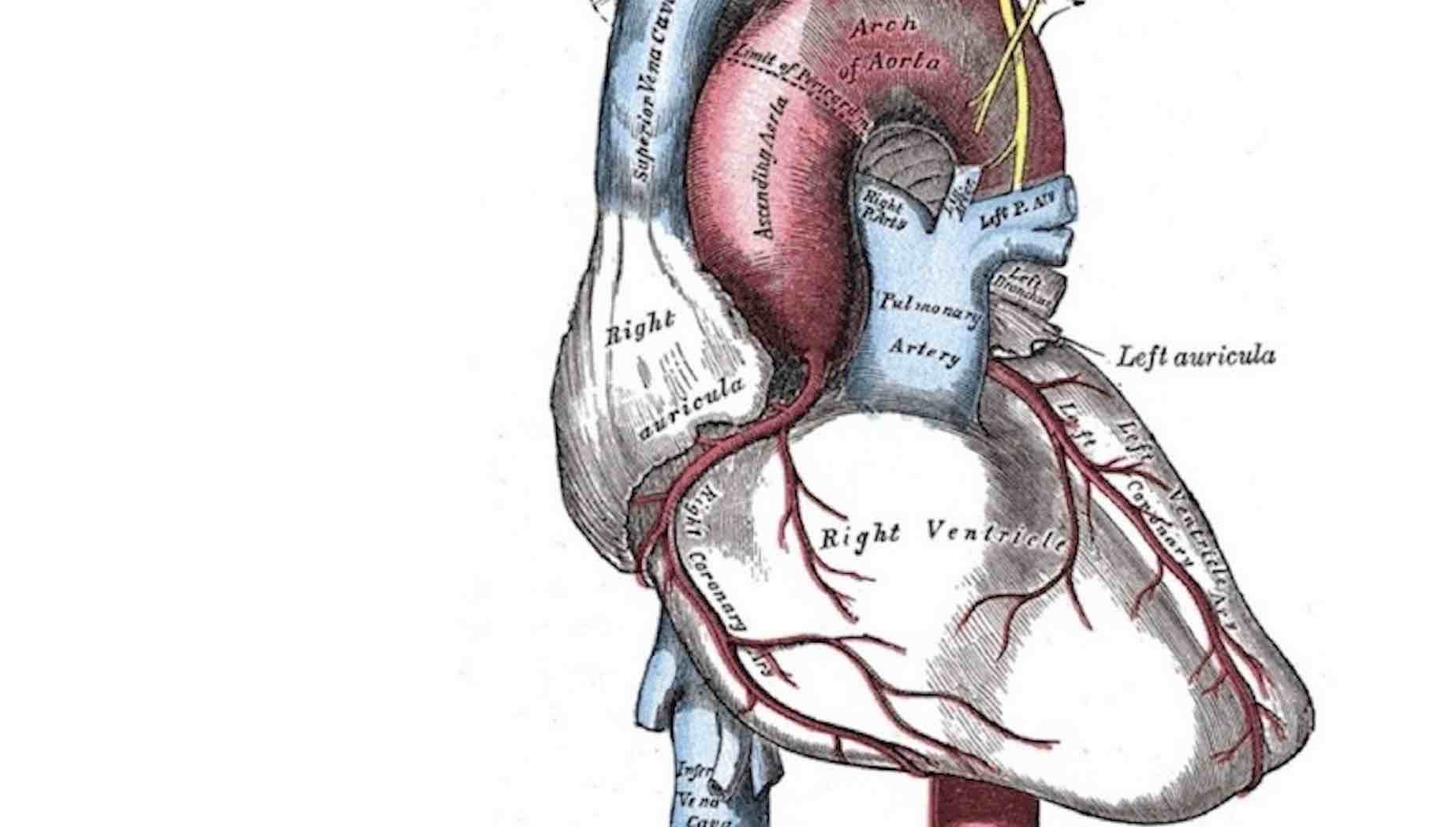
45% of those with heart disease have OSA
OSA has long been known to worsen heart disease. It increases your Cardiovascular (heart attack) and Cerebrovascular (stroke) risk.
OSA and Congenital long QT syndrome (LQTS)
We've long known OSA has been associated with a higher prevalence of AF, and worsening AF control. We now
Don’t forget Depression and OSA!
A poor night's sleep can affect anyone's mental state, and can lead to depression and anxiety. Being excessively sleepy
Recall : Resmed ASV machines could increase mortality risk in heart failure
Central Sleep Apnoea (CSA) in the setting of Heart Failure usually presents with Cheyne Stokes Respiration (CSR) on a
CPAP prevents Atrial Fibrillation (AF) in OSA
Previously we described how those with Obstructive Sleep Apnoea (OSA) have a 4-fold increased risk of Atrial Fibrillation (AF)...
Blue light and Body Clock Problems
Does your body clock feel as though it isn't running at 24hours? Are you sleeping too early, too late,
OSA, poor sleep linked to memory loss
We have long known that a poor night's sleep will impair your memory and concentration, but in recent times
RLS Treatment associated with gambling, Impulse Control Disorders (ICDs)
One of the most common sleep disorders is The Restless Legs Syndrome (RLS), and one of the commonly used
Fixing Sleep in teenagers and adolescents
Sleep problems exist at every age group, and that’s why we’re delighted to remind everyone that we not only
Hypertension (high blood pressure) and OSA : an often overlooked link
There are many reasons why you may have Hypertension (high blood pressure), including genetic reasons, dietary reasons, and cardiac
Parasomnia : Sleepwalking, Sleeptalking
Do you Sleepwalk, Sleeptalk, perhaps sleep-eat, or even hurt yourself or others in the night? This is usually indicative
The cost of untreated OSA to Australians : health, time, and lost productivity
Untreated OSA is associated with a higher risk of heart attacks, strokes, worsening diabetes, and car accidents. Did
Your eyes and OSA
Did you know that OSA can manifest in your eyes? Obstructive Sleep Apnoea (OSA) can contribute to many
Atrial Fibrillation (AF) and OSA
Obstructive Sleep Apnoea (OSA) is associated with diabetes, hypertension, erectile dysfunction, glaucoma, and of course heart disease. One of
Book your Sleep Study